MAS was a proud sponsor of this year’s Hauora Taiwhenua Rural Health Network Conference, where more than 400 medical experts gathered to tackle the challenges and celebrate the wins of a vital part of our nation’s health sector, writes Libby Schultz.
In early 2023, when access to the Coromandel was cut off by the roading collapse, health workers rallied the help of local fishers to deliver prescriptions to people by boat.
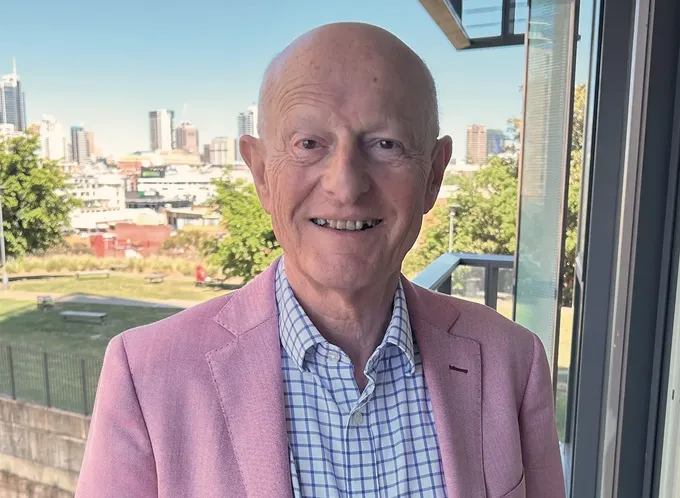
“It’s that kind of can-do spirit that’s the hallmark of rural practice,” says Dr Grant Davidson, CEO of Hauora Taiwhenua Rural Health Network.
“Whatever challenges they face, they still manage to make it work.”
But it will take more than a plucky number-8 wire approach to solve some of the serious problems facing the rural health sector.
Hauora Taiwhenua’s 2024 conference was held in Wellington in early April, and onMAS asked Grant what was top of the agenda – and top of mind – for the 400+ delegates.
Rural communities are now recognised in law
Hauora Taiwhenua was launched in July 2022 when the Rural GP Network partnered with other rural health groups to create a bigger 9-chapter collective – and a united voice.
One of their first big wins was having rural communities recognised as a priority population in the Pae Ora (Healthy Futures) legislation.
“That was an important achievement that’s springboarded all sorts of things over the past 18 months,” says Grant.
Among other things, it’s seen the launch of a new rural telehealth programme, a pilot from Te Whatu Ora to fund the relocation of overseas doctors willing to work in rural areas and funding to send health workers to impacted regions in the aftermath of Cyclone Gabrielle.
“There’s been a lot happening and plenty more to come.”

Rural Health Network Chief Executive Dr Grant Davidson
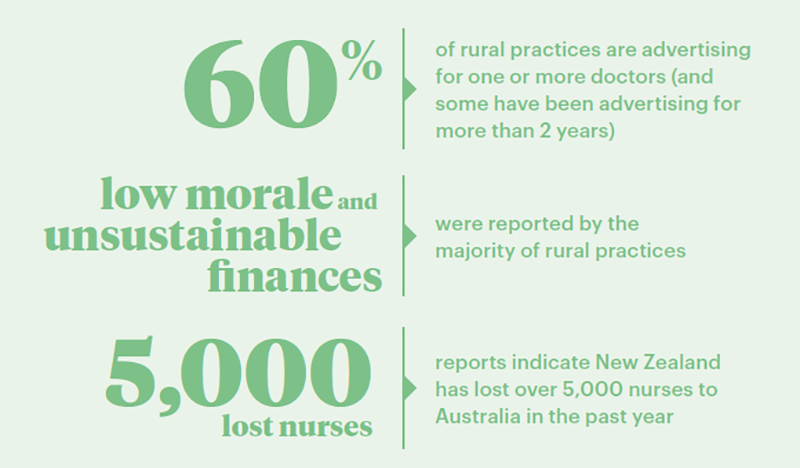
Some of the sobering facts reported by Hauora Taiwhenua.
New medical school to train rural doctors
Another reason to celebrate is the government’s announcement to add a third medical school in New Zealand, with a focus on training rural doctors. A memorandum of understanding has been signed with the University of Waikato, with the first intake of 120 students planned for 2027.
In more good news, Otago and Auckland medical schools will get extra funding to run rural immersion programmes as part of their doctor training.
“These initiatives are great to see,” says Grant. “All the evidence supports the fact that, if people spend time training in rural areas, they’re much more likely to stay practising there.”
While those future initiatives are heartening, the current reality is stark.
Grant says the rural health sector is still operating “under dire stress” with serious workforce shortages.
He says the conference was an opportunity for members to support and bolster each other through the challenges.
Sharing knowledge around climate change
One of the conference themes was resiliency. With rural communities bearing the brunt of recent weather events, conference speakers shared their experiences and learnings.
“We know we’re going to get more of these events – it’s a matter of where and when,” says Grant.
“Every situation will be different and there’s no set playbook. It’s mental preparedness more than anything.”
Last year, Hauora Taiwhenua funded some research into the impacts of climate change on rural practice in Aotearoa. It raised some thought-provoking findings.
“With rising temperatures, we’re likely to see increased risk from things like tropical diseases, water borne illness and heatwave-related deaths,” says Grant.
“As a sector, we need to be thinking about a whole range of climate-related health issues and how we’ll respond.”
The game-changing power of technology
Technology was another key theme at the conference, encompassing some exciting things on the horizon such as the massive productivity potential of artificial intelligence (AI) as well as some persistent real-world problems.
“We did a recent survey that showed a number of our practices still don’t have high-speed internet, and only 74% of rural families have internet in their homes,” says Grant.
And while telehealth is seen as an important future tool for rural communities, it relies on patients having connectivity.
“If some of those people can’t access or afford the data or devices, we’ll still have massive inequities.”
An inspiring example of a community tackling this very challenge is Te Aka Toitū’s Connected Project.
By using a tower installed at the local school to transmit free Wi-Fi into homes, they’re helping to close the digital divide for Eastern Bay of Plenty low-decile school students and their families. It’s having a positive impact on both health outcomes and employment opportunities in the region.
“That’s another great example of the innovative thinking and can-do spirit that exists in rural communities,” says Grant.
Know someone who might enjoy this?
Read this next
-
November 2022
The world needs your work
-
March 2023
Ancient wisdom, modern workplace
-
August 2023
How 2023 will change the landscape of insurance
-
November 2023
The emotional equation of retirement planning
Professional life
See all-
March 2021
Made for today a century ago
-
March 2021
The great brain gain
-
March 2021
A hectic, horrific working holiday
-
March 2021
Smooth sailing for Southern Spars